In this article, we will explore the progression of congestive heart failure (CHF) and discuss the four stages that individuals may experience. We will provide an overview of each stage, including the symptoms, management, and treatment options available. Understanding the stages of CHF is crucial for both patients and healthcare providers to ensure proper diagnosis, treatment, and management of this condition.
Congestive heart failure stages are classified based on the severity of the condition and help determine the appropriate treatment plan. By identifying the stage of CHF, physicians can provide personalized care to improve the patient’s quality of life and slow down the progression of the disease.
Throughout this article, we will delve into each stage of congestive heart failure, starting from the early stages where individuals are at risk, to the later stages where their condition becomes more severe. We will also discuss the management and treatment options available for each stage, allowing patients to make informed decisions about their healthcare.
Join us as we explore the stages of congestive heart failure and gain valuable insights into managing and treating this condition effectively.
Introduction to Congestive Heart Failure (CHF)
Congestive heart failure (CHF) is a chronic condition that affects the heart’s ability to pump blood efficiently. It occurs when the heart muscles are weakened or damaged, preventing the heart from adequately supplying oxygen and nutrients to the body’s organs and tissues. CHF is a progressive condition that can develop gradually or occur suddenly, and it requires medical attention and ongoing management.
There are several factors that can contribute to the development of congestive heart failure. One of the primary causes is coronary artery disease, which occurs when the blood vessels that supply the heart become narrow or blocked, restricting blood flow. Other conditions, such as high blood pressure, heart valve disorders, and heart muscle diseases, can also lead to the weakening of the heart muscles and the onset of CHF.
In addition to these underlying causes, certain lifestyle factors can increase the risk of developing congestive heart failure. These include smoking, obesity, a sedentary lifestyle, and a diet high in saturated fats and cholesterol. It’s important to understand that while these factors can contribute to the development of CHF, they are not the sole causes.
Early detection and timely treatment are crucial in managing congestive heart failure. In the next sections, we will delve into the four stages of CHF, exploring the symptoms, management strategies, and treatment options available at each stage. By understanding the progression of this condition and implementing appropriate interventions, individuals with congestive heart failure can improve their quality of life and effectively manage their symptoms.
What Are the 4 Stages of Congestive Heart Failure?
Stage 1: At Risk for Congestive Heart Failure
In the first stage of congestive heart failure (CHF), individuals are considered to be at risk for developing the condition. This stage is characterized by the presence of risk factors and early signs of heart dysfunction that may progress to CHF if left untreated.
Common risk factors for stage 1 congestive heart failure include:
- High blood pressure
- Coronary artery disease
- Diabetes
- Obesity
- Smoking
- Family history of heart disease
Symptoms of Stage 1 Congestive Heart Failure
While individuals in stage 1 may not experience significant symptoms, there are notable signs of heart dysfunction that may warrant further evaluation:
- Fatigue
- Shortness of breath, especially during physical exertion
- Swelling in the ankles, feet, and legs
- Increased heart rate
Prognosis for Stage 1 Congestive Heart Failure
The prognosis for individuals in stage 1 of congestive heart failure is generally favorable with early intervention and lifestyle modifications. By managing risk factors and making necessary lifestyle changes, individuals can often delay or prevent the progression of CHF.
Regular medical check-ups, blood pressure control, and adherence to a heart-healthy diet and exercise routine are essential for managing stage 1 CHF. Individuals should also quit smoking, limit alcohol consumption, and manage other underlying medical conditions such as diabetes or high cholesterol.
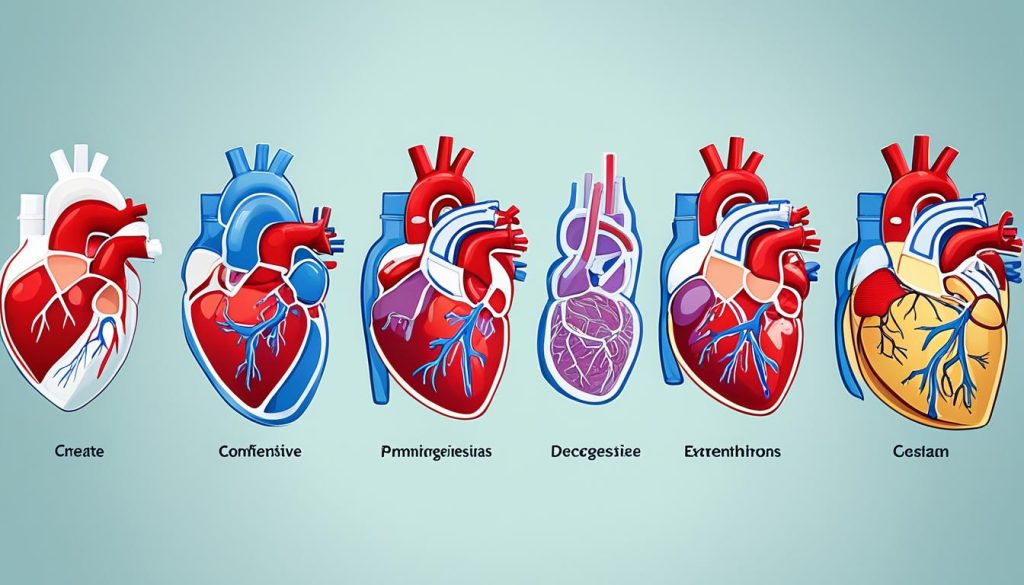
| Stage | Characteristic Features | Symptoms | Treatment Options |
|---|---|---|---|
| Stage 1: At Risk for CHF | Presence of risk factors and signs of heart dysfunction | Fatigue, shortness of breath, swelling, increased heart rate | Lifestyle changes, risk factor management |
| Stage 2: Mild CHF | Progression of heart dysfunction with mild limitations | Worsening fatigue, increased difficulty breathing, reduced exercise capacity | Medications, lifestyle modifications, symptom management |
| Stage 3: Moderate CHF | Significant heart dysfunction with moderate limitations | Severe fatigue, frequent shortness of breath, limited physical activity | Medications, heart failure therapies, lifestyle changes |
| Stage 4: Severe CHF | Advanced heart dysfunction with severe limitations | Extreme fatigue, severe shortness of breath, limited mobility | Palliative care, advanced heart failure management, heart transplant |
Stage 2: Mild Congestive Heart Failure
Mild congestive heart failure (CHF), also known as stage 2 CHF, represents a significant progression in the disease. At this stage, the heart’s ability to pump blood efficiently becomes impaired, leading to noticeable symptoms and increased medical attention.
Symptoms:
- Shortness of breath, particularly during physical activity
- Fatigue and weakness
- Swelling in the ankles, feet, or legs
- Increased heart rate
- Reduced ability to exercise
Progression:
Without proper management, stage 2 CHF can progress to more severe stages. It is crucial to understand the progression of the disease to ensure timely interventions and prevent further deterioration.
Implications of the Diagnosis
Being diagnosed with stage 2 CHF requires individuals to adapt to a new lifestyle and closely monitor their health. It is essential to work closely with healthcare professionals to develop a personalized treatment plan and prevent complications.
Treatment and Management Strategies:
Early intervention and appropriate management are key to slowing down the progression of CHF at this stage. The following strategies are often recommended:
- Medications: Your healthcare provider may prescribe medications to help control symptoms, reduce fluid buildup, and improve heart function.
- Lifestyle modifications: Adopting a heart-healthy lifestyle can have a significant impact. This includes maintaining a balanced diet, engaging in regular physical activity as tolerated, managing stress levels, and avoiding smoking or excessive alcohol consumption.
- Monitoring and follow-ups: Regular monitoring of symptoms and frequent appointments with your healthcare provider are crucial to monitor disease progression and adjust treatment plans accordingly.
- Cardiac rehabilitation: Enrolling in a cardiac rehabilitation program can provide guidance on exercise routines, education on managing the disease, and emotional support.
By implementing these strategies, individuals with mild CHF can optimize their quality of life and potentially delay the progression to more severe stages.
Managing stage 2 CHF requires a holistic approach that includes the support of healthcare professionals, lifestyle modifications, and consistent adherence to the prescribed treatment plan. Through proactive management, individuals with mild CHF can effectively navigate their condition and maintain a fulfilling life.
Stage 3: Moderate Congestive Heart Failure
In stage 3 of congestive heart failure (CHF), individuals experience a moderate level of severity. At this stage, the heart’s ability to pump blood becomes significantly impaired, leading to noticeable symptoms that affect daily life.
Common symptoms of moderate CHF include:
- Shortness of breath, especially during physical activity
- Fatigue and weakness
- Fluid retention, leading to swelling in the legs, ankles, and feet
- Difficulty sleeping, often due to a persistent cough or wheezing
- Reduced ability to exercise or engage in physical activities
The impact of stage 3 CHF on an individual’s daily life can be quite significant. Everyday activities such as walking, climbing stairs, or even getting dressed may become challenging and exhausting. As a result, individuals may experience a decreased quality of life and limitations in performing routine tasks.
Managing and treating stage 3 CHF involves a multidisciplinary approach. Treatment options aim to alleviate symptoms, slow down the progression of the disease, and improve overall heart function.
Some management strategies and treatment options for stage 3 CHF include:
- Medications: Doctors may prescribe a combination of medications to manage symptoms and improve heart function. These may include diuretics to remove excess fluid, ACE inhibitors or angiotensin receptor blockers to relax blood vessels, and beta-blockers to reduce the workload on the heart.
- Lifestyle modifications: Making necessary lifestyle changes can greatly benefit individuals with stage 3 CHF. These changes may include adopting a heart-healthy diet, incorporating regular exercise within the limits of the condition, monitoring fluid intake, and avoiding activities or substances that can worsen symptoms.
- Cardiac rehabilitation: Participating in a structured cardiac rehabilitation program can assist individuals in managing their condition. These programs provide personalized exercise plans, education on heart-healthy habits, and emotional support.
- Devices and procedures: In some cases, certain devices or procedures may be recommended to improve heart function. These may include implantable cardioverter defibrillators (ICDs) to regulate heart rhythms, cardiac resynchronization therapy (CRT) to coordinate heart contractions, or ventricular assist devices (VADs) to support heart function in advanced cases.
- Regular medical follow-up: Regular check-ups with healthcare providers are crucial for monitoring the progression of CHF and adjusting treatment plans as needed.
By effectively managing stage 3 CHF, individuals can improve their symptoms, maintain a better quality of life, and potentially slow down the progression to more severe stages of the disease.
Comparison of CHF Stages
| CHF Stage | Description | Symptoms | Treatment Options |
|---|---|---|---|
| Stage 1 | At risk for CHF | Asymptomatic | Lifestyle changes, medication as needed |
| Stage 2 | Mild CHF | Mild symptoms during physical exertion | Lifestyle changes, medication |
| Stage 3 | Moderate CHF | Significant symptoms affecting daily life | Medication, lifestyle modifications, cardiac rehabilitation, devices/procedures as needed |
| Stage 4 | Severe CHF | Severe symptoms at rest | Medication, lifestyle modifications, devices/procedures, palliative/hospice care as needed |
Stage 4: Severe Congestive Heart Failure
In the final stage of congestive heart failure, known as stage 4, individuals experience severe symptoms and face significant challenges. At this stage, the heart’s ability to pump blood efficiently is severely compromised, leading to a decline in overall health and quality of life.
Common symptoms experienced in stage 4 include severe fatigue, shortness of breath even at rest, fluid accumulation in the lungs and other parts of the body, and frequent hospitalizations for heart-related complications. The severity of symptoms often necessitates continuous medical support and intensive care.
Prognosis and life expectancy in stage 4 congestive heart failure vary depending on several factors, including the individual’s overall health, the effectiveness of treatment, and the presence of other underlying medical conditions. While it is difficult to predict an exact time frame, in some cases, individuals with stage 4 CHF may have a life expectancy of less than a year.
Treatment options in stage 4 concentrate on managing symptoms and improving the individual’s comfort. These may include medications to alleviate fluid buildup, diuretics to control swelling, and palliative care to enhance quality of life. End-of-life considerations, such as advanced directives and hospice care, are also important aspects that individuals and their loved ones should discuss with healthcare providers.
Treatment options for Stage 4 Congestive Heart Failure
To address the severe symptoms and challenges faced in stage 4 congestive heart failure, healthcare providers focus on a multidisciplinary approach. Treatment options can include:
- Medications: Using a combination of medications to manage symptoms and improve heart function, including beta-blockers, ACE inhibitors, and aldosterone antagonists.
- Device therapy: Implanting devices such as pacemakers or implantable cardioverter-defibrillators (ICDs) to help regulate heart rhythm and prevent sudden cardiac arrest.
- Heart transplant: In some cases, heart transplantation may be considered for individuals with end-stage heart failure.
- Palliative care: Providing comprehensive support to improve quality of life, manage symptoms, and address emotional and psychological needs.
It is important for individuals with stage 4 congestive heart failure to work closely with their healthcare team to develop a personalized treatment plan that addresses their unique needs and goals. Regular monitoring, follow-up visits, and open communication with healthcare providers are crucial in managing this advanced stage of the disease.
Management and Treatment of Congestive Heart Failure in Each Stage
Effective management and treatment play a crucial role in improving the quality of life for individuals with congestive heart failure (CHF) at every stage. By implementing a comprehensive approach that combines lifestyle modifications, medications, and other interventions, healthcare professionals can help patients slow down the progression of the disease and alleviate symptoms.
Stage 1: At Risk for Congestive Heart Failure
During the early stage of CHF, individuals may exhibit signs that indicate an increased risk of developing congestive heart failure. To manage this stage effectively, patients are often advised to make certain lifestyle changes. These may include adopting a heart-healthy diet, engaging in regular exercise, and controlling blood pressure and cholesterol levels. By taking these preventive measures, individuals can reduce the likelihood of progressing to the more advanced stages of the disease.
Stage 2: Mild Congestive Heart Failure
As the disease progresses to stage 2, treatment approaches become more focused on symptom management and slowing down the worsening of heart function. In addition to adhering to a heart-healthy lifestyle, patients may be prescribed medications such as diuretics to reduce fluid buildup and beta-blockers to improve heart function. Regular monitoring and routine follow-ups with healthcare providers are essential to ensure optimal management of symptoms and adjust treatment plans as needed.
Stage 3: Moderate Congestive Heart Failure
In stage 3, the symptoms of congestive heart failure become more pronounced, impacting an individual’s daily life and physical abilities. Management strategies at this stage may involve additional medications, such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), to help relax blood vessels and improve the heart’s efficiency. Healthcare providers may also recommend cardiac rehabilitation programs and specialized exercise regimens to increase endurance and improve overall heart health.
Stage 4: Severe Congestive Heart Failure
In the advanced stage of CHF, treatment focuses on alleviating symptoms, improving quality of life, and providing palliative care. Along with optimal medication management, individuals may require assisted devices such as implanted defibrillators or ventricular assist devices (VADs) to support heart function. In some cases, heart transplantation may be considered as a potential treatment option. Hospice care and end-of-life discussions become important considerations in this stage.
Throughout all stages of congestive heart failure, it is paramount for individuals to maintain open and regular communication with their healthcare team. By closely adhering to treatment plans, making necessary lifestyle adjustments, and actively participating in their own care, individuals can better manage their condition and improve overall outcomes.
Conclusion and Tips for Preventing or Managing Congestive Heart Failure
In conclusion, congestive heart failure (CHF) is a serious condition that progresses through four stages. These stages range from being at risk for CHF to severe heart failure. Each stage has its own set of symptoms and challenges, and management and treatment options vary accordingly.
To prevent or manage CHF, it is crucial to make certain lifestyle changes. This includes adopting a heart-healthy diet, regular exercise, and avoiding smoking and excessive alcohol consumption. Additionally, it is essential to diligently follow the prescribed medications and treatment plans provided by healthcare professionals.
When it comes to recovery, the outlook for congestive heart failure depends on various factors such as the stage of the disease, the individual’s overall health, and the effectiveness of treatment. With proper management, some individuals may experience improved symptoms and quality of life. However, complete recovery from CHF may not be possible in all cases.
It is important to note that congestive heart failure and heart failure are often used interchangeably. However, there is a slight difference in their definitions. Congestive heart failure specifically refers to a condition where fluid builds up in the body due to a weakened heart, while heart failure is a broader term that encompasses various conditions that affect the heart’s ability to pump blood effectively.