Endometrial hyperplasia, a precancerous condition of the uterine lining, raises concerns about the risk of developing endometrial cancer. Individuals diagnosed with endometrial hyperplasia often wonder how long it takes for this condition to progress into cancer. The progression from endometrial hyperplasia to cancer is a stepwise process that can take several years. It is essential to understand the factors influencing this progression and the importance of monitoring and timely treatment.
Endometrial hyperplasia occurs when there is an imbalance of estrogen and progesterone hormones, resulting in the growth of abnormal cells in the uterine lining. Most cases of endometrial hyperplasia start as simple thickening of the uterine lining but can develop into more advanced stages if left untreated. The risk of progression to cancer is higher in cases of atypical hyperplasia compared to non-atypical hyperplasia.
To prevent the development of endometrial cancer, regular monitoring and appropriate treatment are crucial. By addressing risk factors, such as being overweight or having certain medical conditions, individuals can reduce their chances of developing endometrial hyperplasia. Early detection of any changes in the uterine lining through regular ultrasounds and biopsies can help detect progression to cancer at an early stage.
By staying proactive and vigilant, individuals with endometrial hyperplasia can minimize the risk of progression to cancer and promote their overall health and well-being. In the following sections, we will explore the risk factors for endometrial hyperplasia, the stages of this condition, monitoring and treatment options, the timeline of progression to cancer, and the importance of early detection in improving outcomes.
Risk Factors for Endometrial Hyperplasia
Several factors can increase the risk of developing endometrial hyperplasia. It is important to address these risk factors to reduce the likelihood of developing this precancerous condition.
Endometrial hyperplasia is a precancerous condition characterized by the abnormal growth of cells in the uterine lining. If left untreated, it can progress to endometrial cancer.
Common Risk Factors for Endometrial Hyperplasia
1. Being overweight: Obesity is a significant risk factor for developing endometrial hyperplasia. Excess body fat can lead to higher estrogen levels, which can disrupt the hormonal balance and increase the risk of abnormal cell growth.
2. Diabetes mellitus: Women with diabetes have an increased risk of developing endometrial hyperplasia. Insulin resistance and high insulin levels can promote cell growth in the uterus.
3. Polycystic ovarian syndrome (PCOS): PCOS is a hormonal disorder that causes irregular periods and an imbalance of estrogen and progesterone. These hormonal imbalances can contribute to the development of endometrial hyperplasia.
4. Taking estrogen supplements without progesterone: Estrogen therapy without the addition of progesterone can lead to an increased risk of endometrial hyperplasia. Progesterone helps counteract the effects of estrogen on the uterine lining.
List of Risk Factors:
- Being overweight
- Diabetes mellitus
- Polycystic ovarian syndrome (PCOS)
- Taking estrogen supplements without progesterone
By understanding and addressing these risk factors, individuals can take proactive steps to reduce their chances of developing endometrial hyperplasia. Lifestyle modifications, such as maintaining a healthy weight, managing diabetes, and discussing hormone therapy options with a healthcare provider, can help mitigate the risk.
Stages of Endometrial Hyperplasia
Endometrial hyperplasia, a precancerous condition, can be classified into different stages based on the severity of abnormal cell growth in the uterine lining. Understanding the stages of endometrial hyperplasia helps determine the appropriate treatment approach.
1. Simple Endometrial Hyperplasia
Simple endometrial hyperplasia is a mild form of the condition. It involves a slight thickening of the uterine lining and typically has a low risk of progressing to cancer. This stage often resolves with proper treatment and monitoring.
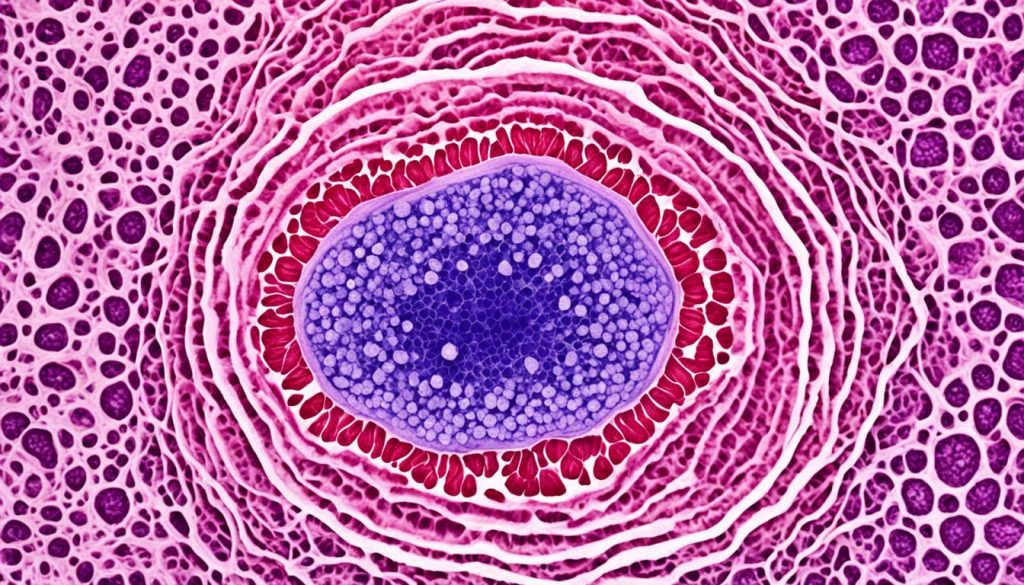
2. Complex Hyperplasia
Complex hyperplasia is a more advanced form of endometrial hyperplasia. It is characterized by the formation of crowded glands in the uterine tissue. Compared to simple hyperplasia, complex hyperplasia poses a higher risk of progressing to cancer.
3. Severely Atypical Endometrial Hyperplasia
Severely atypical endometrial hyperplasia is the highest stage of endometrial hyperplasia. It involves the presence of abnormal glandular cells in the uterine lining. This stage carries the highest risk of progressing to endometrial cancer.
Identifying the stage of endometrial hyperplasia is crucial for determining the appropriate course of treatment. Treatment options may include hormonal therapy or surgical interventions, depending on factors such as age, desire for future pregnancies, and the severity of the condition.
By addressing endometrial hyperplasia at an early stage and following recommended treatments, individuals can help prevent the progression to endometrial cancer and maintain their health and well-being.
Monitoring and Treatment of Endometrial Hyperplasia
Regular monitoring is essential for women diagnosed with endometrial hyperplasia to detect any changes or progression to cancer. This typically involves regular ultrasounds of the uterus and biopsies of the uterine lining
The treatment for endometrial hyperplasia depends on various factors such as age, desire for future pregnancies, and the severity of the condition. Surgical options include hysterectomy (removal of the uterus and cervix) for more severe cases or hormone therapy for those who wish to avoid surgery. Hormone therapy involves the use of progestin to reverse the effects of estrogen on the uterine lining. Monitoring and appropriate treatment can help prevent the development of endometrial cancer.
| Treatment | Advantages | Disadvantages |
|---|---|---|
| Surgical Options (Hysterectomy) | – Removes the uterus and cervix, eliminating the risk of endometrial cancer – Suitable for women who have completed childbearing – Resolves symptoms of endometrial hyperplasia |
– Involves surgery and recovery time – Not applicable for women who wish to preserve fertility |
| Hormone Therapy (Progestin) | – Non-surgical option – Reverses the effects of estrogen on the uterine lining – Can be used for women who wish to preserve fertility |
– May have side effects such as irregular bleeding or breast tenderness – Requires regular monitoring and follow-up |
Benefits of Regular Monitoring
- Allows for early detection of any changes or progression to cancer
- Provides an opportunity to assess the effectiveness of treatment
- Enables timely adjustments to the treatment plan, if necessary
- Offers peace of mind and reassurance for patients
By closely monitoring endometrial hyperplasia and providing appropriate treatment, healthcare professionals can effectively prevent the development of endometrial cancer and ensure the well-being of individuals affected by this condition.
Progression of Endometrial Hyperplasia to Cancer
The progression of endometrial hyperplasia to cancer can vary depending on the stage of the hyperplasia and individual factors. Atypical hyperplasia, the highest stage of endometrial hyperplasia, has a higher risk of progression to cancer compared to non-atypical hyperplasia. Studies have shown that the risk of progression among women with atypical hyperplasia is around 8% through four years, rising to 28% through 19 years of follow-up. Non-atypical forms of endometrial hyperplasia are less likely to progress to cancer. Early detection and appropriate treatment can help prevent the progression of endometrial hyperplasia to cancer.
Progression Risk of Endometrial Hyperplasia
| Stage of Endometrial Hyperplasia | Risk of Progression to Cancer |
|---|---|
| Atypical Hyperplasia | 8% through four years 28% through 19 years of follow-up |
| Non-Atypical Hyperplasia | Less likely to progress to cancer compared to atypical hyperplasia |
Early Detection of Endometrial Cancer
Early detection plays a crucial role in improving outcomes for women with endometrial hyperplasia, who are at an increased risk of developing endometrial cancer. Regular monitoring and follow-up appointments with healthcare professionals are essential for detecting any signs or symptoms of cancer at an early stage.
One of the key diagnostic tools used in the early detection of endometrial cancer is regular ultrasound scans. These scans can provide valuable information about the thickness and texture of the uterine lining, helping healthcare professionals identify any abnormalities or changes that may indicate cancerous growth.
Another important diagnostic procedure for early detection is an endometrial biopsy. This involves the removal of a small tissue sample from the lining of the uterus, which is then examined under a microscope for the presence of cancer cells. Endometrial biopsies are typically performed on an outpatient basis and are relatively quick and minimally invasive.
Women with endometrial hyperplasia should be vigilant about any changes in their health and seek medical attention if they experience abnormal bleeding, pelvic pain, or other concerning symptoms. Prompt reporting of symptoms and regular check-ups can significantly improve the chances of early detection and successful treatment.

Signs and Symptoms to Watch Out For:
- Abnormal vaginal bleeding, including heavy or prolonged periods
- Postmenopausal bleeding
- Pelvic pain or discomfort
- Unexplained weight loss
- Feeling of fullness in the pelvic area
If you experience any of these symptoms or have concerns about your reproductive health, it is crucial to consult with a healthcare professional as soon as possible. Remember, early detection of endometrial cancer can greatly increase the chances of successful treatment and improved outcomes.
Prognosis and Treatment Options for Endometrial Hyperplasia
When it comes to endometrial hyperplasia, the prognosis and treatment options vary depending on several factors. These include the stage of the hyperplasia and the individual’s response to treatment.
Simple endometrial hyperplasia typically has a more favorable prognosis compared to complex or atypical hyperplasia. It is important to note that atypical hyperplasia carries a higher risk of progression to cancer compared to non-atypical hyperplasia.
In terms of treatment options, there are two main approaches: hormone therapy and surgical intervention. Hormone therapy involves the use of progestin to reverse the effects of estrogen on the uterine lining. This treatment option is often recommended for women who wish to preserve their fertility. On the other hand, surgical interventions, such as a hysterectomy (removal of the uterus and cervix), may be considered for more severe cases or for those who no longer wish to have children.
The choice of treatment depends on various factors, including age, desire for future pregnancies, and the severity of the condition. Consultation with a healthcare professional is crucial to determine the most appropriate and individualized treatment plan.
To illustrate the differences between the treatment options, here is a detailed table:
| Treatment Option | Advantages | Considerations |
|---|---|---|
| Hormone Therapy |
|
|
| Surgical Intervention (Hysterectomy) |
|
|
Regular follow-up appointments and monitoring are essential to ensure the effectiveness of the chosen treatment and to detect any potential recurrence or progression. By working closely with healthcare professionals, individuals with endometrial hyperplasia can receive the care they need for optimal outcomes.
Conclusion
Endometrial hyperplasia is a precancerous condition that poses a risk of progression to endometrial cancer if left untreated. Individuals diagnosed with endometrial hyperplasia should be proactive in their approach to monitoring and treatment. Regular follow-up appointments with healthcare professionals are essential for early detection of any changes or signs of endometrial cancer.
Early detection plays a crucial role in improving outcomes for individuals with endometrial hyperplasia. By promptly addressing any abnormal symptoms or concerns, individuals can significantly reduce their risk of the condition progressing to cancer. Timely interventions, such as hormone therapy or surgery, can be effective in preventing the development of endometrial cancer.
Monitoring endometrial hyperplasia and seeking appropriate treatment options are key strategies for minimizing the cancer risk associated with this condition. Being proactive and well-informed empowers individuals to take control of their health and well-being. Stay vigilant, attend regular check-ups, and work closely with healthcare professionals to ensure the early detection of endometrial cancer and optimal treatment outcomes.