When faced with a perforated bowel, immediate medical intervention is essential to prevent complications and improve prognosis. But how long can you live with a perforated bowel without surgery? Let’s explore the survival rates, prognosis, and life expectancy of untreated bowel perforation.
Untreated perforated bowel comes with significant risks and complications. Without timely medical intervention, the condition can lead to severe infections, sepsis, and even death. It’s crucial to understand the potential consequences of not seeking emergency treatment.
The survival rate and life expectancy for untreated bowel perforation are significantly lower compared to those who undergo surgical intervention. The longer the perforation goes untreated, the higher the risk of complications and adverse outcomes.
While individual circumstances and disease status can influence prognosis, it is important to recognize the symptoms of a perforated bowel and seek immediate medical care. Timely diagnosis and treatment are vital to improve the chances of survival and minimize the risk of complications.
In the following sections, we will explore the causes, symptoms, complications, diagnostic methods, treatment options, and surgical versus non-surgical outcomes of bowel perforation. Understanding these aspects can help you make informed decisions about your healthcare and ensure prompt intervention when needed.
Stay tuned for the upcoming sections of this article as we delve deeper into the intricacies of bowel perforation and equip you with the knowledge to navigate this critical condition effectively.
Causes of Bowel Perforation
Bowel perforation can occur due to various causes, including spontaneous occurrences, medical procedures, and traumatic events.
Spontaneous Bowel Perforation
Spontaneous bowel perforation can be attributed to underlying medical conditions such as inflammatory bowel disease (IBD). These conditions weaken the intestinal walls, making them more susceptible to rupture and perforation.
Medical Procedure-Related Bowel Perforation
In some cases, bowel perforation can occur as a complication of medical procedures. Surgical interventions, such as colonoscopies or surgeries involving the gastrointestinal tract, carry a small risk of unintentional bowel perforation.
Traumatic Bowel Perforation
Trauma or injury to the bowel can cause perforation. Blunt force trauma or penetrating injuries, such as those sustained in car accidents or violent incidents, can result in bowel perforation.
Other Causes
There are additional factors that can contribute to bowel perforation. These include:
- Tumors in the intestine: Cancerous or non-cancerous tumors can exert pressure on the intestinal walls, leading to perforation.
- Chemotherapy drugs: Certain chemotherapy medications can weaken the intestinal lining, making it more prone to perforation.
- Radiation therapy: High-dose radiation therapy targeting the abdominal area can cause bowel perforation in some cases.
- Blockages: Obstructions in the gastrointestinal tract, such as strictures or intestinal adhesions, can increase the risk of perforation.
- Non-cancerous diseases: Conditions like diverticulitis or ischemic bowel disease can impair blood flow to the intestines, increasing the likelihood of perforation.
Understanding the causes of bowel perforation is vital for early recognition and appropriate medical intervention to minimize complications and improve patient outcomes.
Symptoms and Signs of Bowel Perforation
Bowel perforation can manifest with various symptoms that indicate a medical emergency. Recognizing these signs is crucial for prompt medical intervention. The following are some common symptoms of a perforated bowel:
- Severe abdominal pain: The most noticeable symptom is intense and persistent abdominal pain. It may be localized or spread throughout the abdomen.
- Stomach cramps: Cramping or spasms in the stomach are often present, causing discomfort and distress.
- Bloating: The abdomen may appear distended or swollen, indicating the presence of excess gas or fluid.
- Nausea and vomiting: Feeling sick to the stomach and vomiting are common symptoms of bowel perforation.
- Changes in bowel movements: Bowel habits may change, resulting in diarrhea or constipation.
- Bleeding from the rectum: Blood in the stool or bleeding from the rectum is a concerning symptom that warrants immediate attention.
- Fever and chills: Infections associated with bowel perforation can lead to fever and chills as the body tries to fight the infection.
- Fatigue: Feeling weak, tired, and exhausted can be a sign of a perforated bowel, especially when accompanied by other symptoms.
If you experience any of these symptoms, it is crucial to seek immediate medical attention. Bowel perforation is a serious condition that requires urgent evaluation and treatment to prevent complications and improve outcomes.

Complications of Untreated Bowel Perforation
If left untreated, bowel perforation can lead to serious complications such as infection, sepsis, bleeding, and death. The risk of complications increases with time, and immediate medical intervention is crucial to prevent these adverse outcomes.
Untreated perforated bowel poses significant risks to the patient’s health and well-being. One of the most common complications is infection. When the bowel is perforated, bacteria from the intestine can leak into the abdominal cavity, leading to peritonitis, a severe infection of the peritoneum. This can rapidly progress to sepsis, a life-threatening condition characterized by a systemic inflammatory response to infection.
Another complication of untreated bowel perforation is bleeding. The perforation site may cause ongoing internal bleeding, which can result in anemia and further compromise the patient’s condition. In some cases, the bleeding may be severe and require immediate intervention.
Delayed treatment of a perforated bowel can also increase the risk of postoperative complications if surgery becomes necessary. The longer the bowel remains perforated, the more extensive the damage to the surrounding tissues and structures, making the surgical repair more complex and challenging.
Additionally, untreated bowel perforation can lead to necrosis (tissue death) of the bowel wall. This can cause a segment of the intestine to become nonviable and require removal during surgery. The loss of a significant portion of the intestine can lead to long-term digestive problems and may require further medical interventions, such as the creation of a stoma.
In severe cases of untreated bowel perforation, the risk of death is substantial. The infection, sepsis, and multiorgan failure associated with an untreated perforated bowel can be fatal if left unaddressed.
In conclusion, timely medical intervention is crucial when dealing with bowel perforation to prevent the complications mentioned above and improve the chances of a successful recovery. Seeking immediate medical attention at the first signs and symptoms of bowel perforation is essential for optimal outcomes.
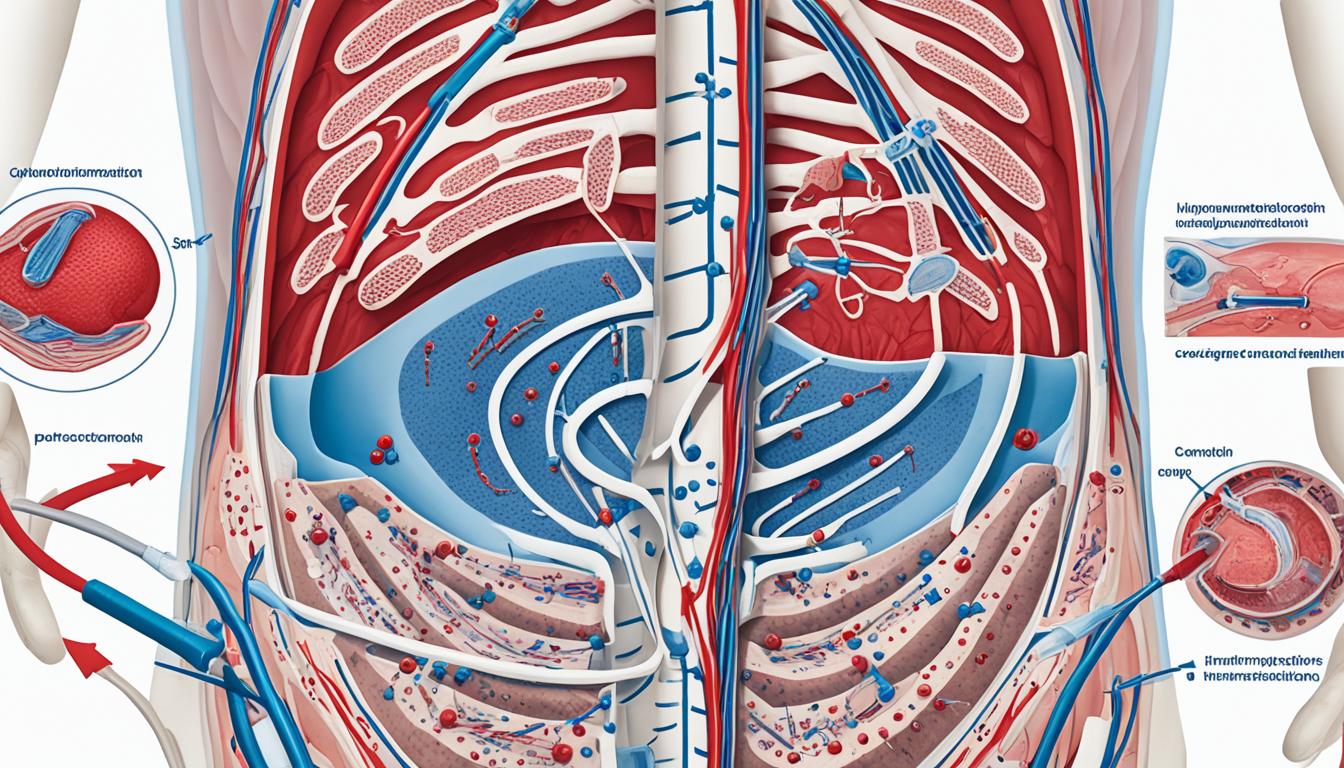
Diagnosis of Bowel Perforation
Diagnosing a perforated bowel involves a comprehensive assessment that combines a physical examination, medical history review, and various diagnostic tests. These tests help identify the presence and location of the perforation, enabling healthcare professionals to determine the most appropriate treatment plan.
During the physical examination, the healthcare provider will carefully assess the patient’s abdomen for signs of tenderness, distension, and abnormal sounds. They will also inquire about the patient’s symptoms and medical history, paying close attention to any previous abdominal surgeries, underlying health conditions, or treatments that might increase the risk of bowel perforation.
To confirm the diagnosis and pinpoint the location of the perforation, several tests may be ordered:
- X-rays: A standard X-ray of the abdomen can help identify signs of bowel perforation, such as air or fluid trapped inside the abdominal cavity.
- CT scans: Computed tomography (CT) scans provide detailed images of the abdomen, allowing healthcare professionals to visualize the structure of the intestines and detect any abnormalities, including perforations.
- Blood tests: Blood tests can help assess the patient’s overall health and identify any signs of infection or inflammation, which may indicate a bowel perforation.
- Endoscopic procedures: Upper gastrointestinal (GI) endoscopy or colonoscopy may be performed to directly visualize the inside of the intestines and identify any perforations or abnormalities.
The combination of these diagnostic measures helps healthcare professionals make an accurate diagnosis, determine the severity of the condition, and plan appropriate treatment for bowel perforation.

| Diagnostic Tests | Purpose | Advantages | Limitations |
|---|---|---|---|
| X-rays | Identify signs of bowel perforation | – Non-invasive | – May not detect all perforations – Limited visualization of internal structures |
| CT scans | Visualize the intestines and detect abnormalities | – Provides detailed images – Accurate detection of perforations |
– Radiation exposure – Cost |
| Blood tests | Assess overall health and detect signs of infection or inflammation | – Simple and widely available | – Non-specific results – Results may require further interpretation |
| Endoscopic procedures | Direct visualization of the intestines | – Allows for direct examination and tissue sampling | – Invasive – Limited accessibility based on the extent of the perforation |
Treatment Options for Bowel Perforation
When it comes to treating a perforated bowel, surgical intervention is the primary and most effective option. In this procedure, a skilled surgeon repairs the hole in the intestine and removes any leaked fluids or waste from the abdomen. Surgical intervention is crucial in preventing further complications and improving the patient’s prognosis.
However, there may be instances where surgical treatment is not feasible, especially for individuals who are not in optimal health. In such cases, non-surgical management of bowel perforation may be considered. This approach involves careful monitoring of the patient’s condition, along with the use of appropriate drainage to aid in the healing process.
While surgical intervention remains the gold standard for treating bowel perforation, non-surgical management can be a viable alternative for individuals who cannot undergo surgery. It is important to consult with a healthcare professional to determine the most appropriate treatment option based on the patient’s specific circumstances.

How Long Can You Live With Perforated Bowel Without Surgery?
When it comes to bowel perforation, the prognosis and life expectancy without surgery are significantly lower compared to surgical intervention. Untreated bowel perforation can lead to severe complications and a higher risk of mortality. The exact life expectancy varies depending on factors such as disease status, individual health, and time to diagnosis and treatment.
Without surgical intervention, the survival rates for bowel perforation decrease dramatically. Studies have shown that the mortality rate for patients with untreated bowel perforation can be as high as 50%. The longer the condition remains untreated, the higher the risk of complications and the lower the chances of survival.
Complications of untreated bowel perforation can include infection, sepsis, abscess formation, peritonitis, and organ failure. These complications can further increase the risk of mortality and have a significant impact on the individual’s quality of life.
In cases where surgery is not performed, the individual’s overall health and the presence of underlying conditions play a crucial role in determining life expectancy. Patients with pre-existing comorbidities or compromised immune systems may have a poorer prognosis without surgical intervention.
Factors Affecting Life Expectancy and Prognosis
The following factors can influence the life expectancy and prognosis for individuals with untreated bowel perforation:
- Time to Diagnosis: Delayed diagnosis can lead to a worsened prognosis, as the condition can progress rapidly without immediate intervention.
- Disease Status: The underlying cause of the bowel perforation, such as inflammatory bowel disease or cancer, can impact overall health and survival rates.
- Individual Health: The individual’s overall health and immune system strength can affect their ability to fight off infections and recover from complications.
- Age: Advanced age can be a contributing factor to a poorer prognosis, as older adults may have weaker immune systems and reduced resilience.
It is important to note that the information provided here is based on studies and medical knowledge. Each case may vary, and it is crucial to consult with a healthcare professional for proper diagnosis and individualized treatment options.
Early Detection and Prompt Medical Attention
Due to the serious nature of bowel perforation and its potential complications, early detection and prompt medical attention are vital. It is crucial to seek immediate medical care if any symptoms of bowel perforation are present, such as severe abdominal pain, vomiting, fever, or changes in bowel movements.
An accurate diagnosis and timely intervention can significantly improve the prognosis and increase the chances of a successful recovery. Diagnostic tests, such as X-rays, CT scans, and blood tests, can help confirm the presence of bowel perforation and guide appropriate treatment.
While surgical intervention is the primary treatment option, non-surgical management may be considered for individuals who are not suitable candidates for surgery. Non-surgical approaches, such as close monitoring and drainage, can help manage the condition and promote healing in selected cases.
It is essential to prioritize one’s health and seek professional medical advice when faced with potential bowel perforation or any concerning symptoms. The collaboration between the patient and healthcare provider is critical in determining the most appropriate treatment plan and optimizing outcomes.
| Factors Affecting Prognosis | Impact on Life Expectancy |
|---|---|
| Disease status | Varies depending on the underlying cause and its progression. |
| Time to Diagnosis | Delayed diagnosis can lead to rapid disease progression and worsen prognosis. |
| Individual health and underlying conditions | Weaker immune systems or comorbidities may contribute to a poorer prognosis. |
| Age | Advanced age can be a contributing factor to a poorer prognosis. |

Conclusion
Living with a perforated bowel is a serious and potentially life-threatening situation. The risks of untreated perforated bowel should not be underestimated, as it can lead to severe complications and even death. It is crucial to recognize the symptoms of bowel perforation, such as severe abdominal pain, bloating, and changes in bowel movements, and seek immediate medical attention if they occur.
Untreated bowel perforation can result in severe infections, including sepsis, which can be life-threatening. The longer the condition remains untreated, the higher the risk of developing complications. Therefore, timely medical intervention and surgical treatment are crucial to improve outcomes and prevent further health complications.
In conclusion, if you suspect that you may be living with a perforated bowel, it is essential to prioritize your health and seek immediate medical care. By recognizing the risks of untreated perforated bowel and understanding the potential complications, you can take proactive steps to ensure the best possible outcome. Follow the recommended treatment plan and work closely with your healthcare provider for a comprehensive approach to managing this critical condition.