Did you know that in the United States alone, an estimated 900,000 people are affected by blood clots each year, resulting in 60,000 to 100,000 deaths? That’s a staggering number, highlighting the seriousness of this condition. When a blood clot forms in the leg, it can potentially travel to the lungs, causing a life-threatening condition called pulmonary embolism. But just how fast does this journey take? Let’s explore the speed at which a blood clot travels from the leg to the lungs and why prompt medical attention is crucial to prevent complications and reduce the risk of death.
What is a Blood Clot and How Does It Form?
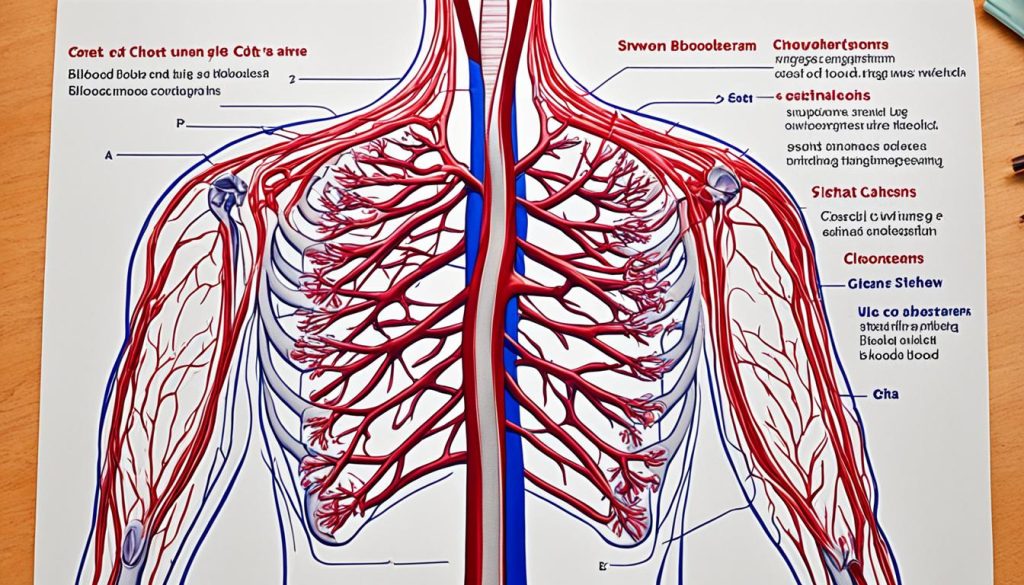
A blood clot, or thrombus, is a solid mass that forms in blood vessels, obstructing the normal flow of blood. It can develop in veins or arteries and is known as venous thromboembolism (VTE) when it occurs in veins. The formation of a blood clot involves various factors, including platelets, clotting proteins, and fibrin. When the blood clot is within a vein in the leg, it is referred to as deep vein thrombosis (DVT). If the clot breaks loose from the leg and travels to the lungs, it can cause a life-threatening condition called pulmonary embolism (PE).
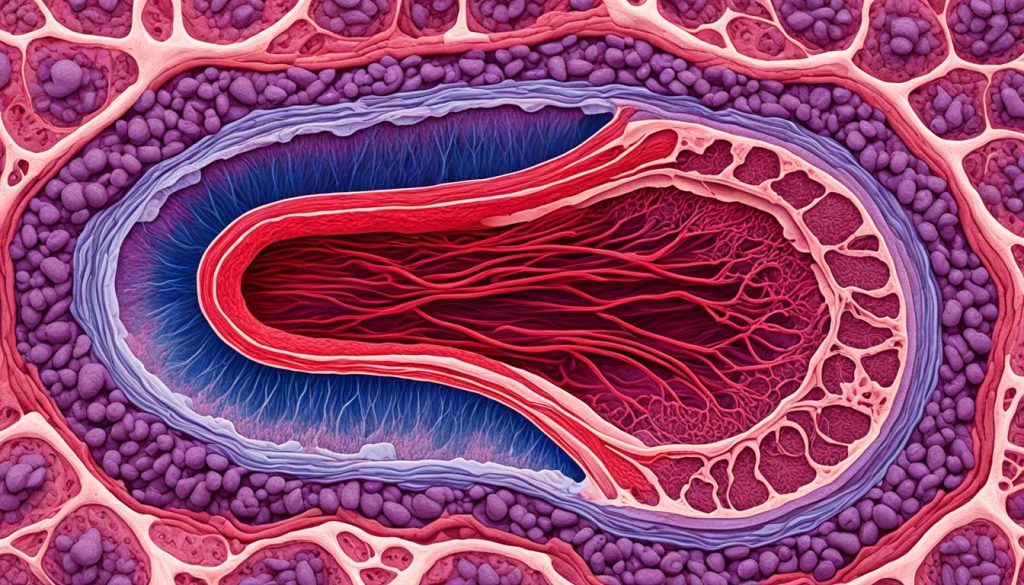
In the process of blood clot formation, several elements come together to create a plug that stops bleeding in damaged blood vessels. When a blood vessel is injured, platelets are activated and begin to stick together, forming a platelet plug. Clotting proteins in the blood, known as clotting factors, then interact with the platelets to reinforce and stabilize the plug. Finally, a protein called fibrin forms a mesh-like network that traps red blood cells and forms a solid clot.
There are different types of blood clots, including arterial clots, which occur in arteries and are commonly associated with cardiovascular diseases, and venous clots, which develop in veins. Venous clots can be further classified into deep vein thrombosis (DVT) and superficial thrombophlebitis. DVT occurs when a clot forms in a deep vein, often in the leg, whereas superficial thrombophlebitis refers to a clot that develops in a vein near the surface of the skin.
The formation of a blood clot is a complex process that plays a vital role in the body’s natural response to injury. However, when a clot forms unnecessarily or obstructs blood flow to vital organs, it can lead to serious health complications. Understanding the formation and types of blood clots is essential for recognizing the signs, seeking timely medical intervention, and preventing further complications.
The Risk Factors for Developing a Blood Clot
There are several factors that increase the risk of developing a blood clot, also known as thrombosis. It is important to be aware of these risk factors and take necessary precautions to prevent blood clots.
1. Personal or Family History
Having a personal or family history of blood clots can predispose an individual to a higher risk of developing future blood clots. If you have a close relative, such as a parent or sibling, who has experienced a blood clot, it is important to inform your healthcare provider.
2. Medical Conditions
Certain medical conditions can increase the risk of blood clot formation. Conditions like heart disease and cancer can disrupt normal blood flow and increase the likelihood of clotting. It is crucial to manage underlying medical conditions and follow your healthcare provider’s recommendations to minimize the risk of blood clots.
3. Surgeries or Trauma
Undergoing surgeries or experiencing trauma can also increase the risk of blood clot formation. When the body undergoes significant surgical procedures or when there is physical trauma, the blood vessels may be damaged, leading to a higher risk of clotting. It is important to follow post-operative care instructions and take appropriate measures to prevent blood clots during the recovery process.
4. Prolonged Periods of Inactivity
Remaining immobile for long periods, such as during long plane flights or extended bed rest, can contribute to blood clot formation. Lack of movement slows down blood circulation and increases the risk of a clot forming. It is advisable to move around and perform simple exercises when in situations that require prolonged periods of inactivity.
5. Smoking and Overweight
Smoking and being overweight are lifestyle factors that can increase the risk of blood clot formation. Smoking damages blood vessels and affects the clotting process, while being overweight puts additional stress on the circulatory system. Quitting smoking and maintaining a healthy weight can significantly lower the risk of blood clots.
6. Medications
Some medications, such as hormone replacement therapy and birth control pills, can increase the risk of blood clot formation. It is important to discuss potential risks and alternatives with your healthcare provider when considering these medications. Your healthcare provider can help determine the most suitable options for managing your health.
Being aware of the risk factors for developing a blood clot is essential for preventing thrombosis. Personal or family history, certain medical conditions, surgeries or trauma, prolonged periods of inactivity, smoking, being overweight, and certain medications are all factors that increase the risk of blood clot formation. By managing these risk factors and taking necessary precautions, individuals can reduce their chances of experiencing a blood clot and its potential complications.
Symptoms of a Blood Clot in the Leg and Lungs
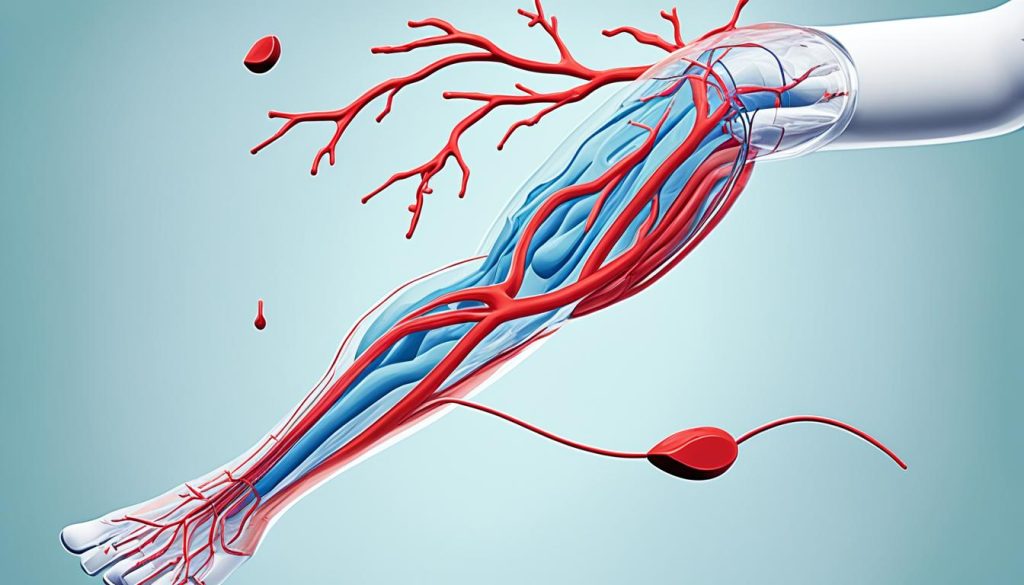
The symptoms of a blood clot in the leg, also known as deep vein thrombosis (DVT), may manifest as:
- Swelling
- Redness
- Darkening or discoloration of the skin
- Pain
- Tenderness
It is important to note that these symptoms are more likely to occur in one leg rather than both.
On the other hand, symptoms of a blood clot in the lungs, known as a pulmonary embolism (PE), include:
- Sudden shortness of breath
- Chest pain that worsens with deep breaths or coughing
- Rapid heart rate
- Cough
- Sometimes fainting
If you experience any of these symptoms, it is crucial to seek immediate medical attention to prevent further complications.
| Leg Blood Clot Symptoms | Lung Blood Clot Symptoms |
|---|---|
| Swelling | Sudden shortness of breath |
| Redness | Chest pain that worsens with deep breaths or coughing |
| Darkening or discoloration of the skin | Rapid heart rate |
| Pain | Cough |
| Tenderness | Sometimes fainting |
How Fast Does a Blood Clot Travel From the Leg to the Lungs?
The speed at which a blood clot travels from the leg to the lungs can vary. While it may take several days or weeks for a clot to reach the lungs in some cases, in others, it can happen within minutes or hours. The exact timeframe depends on factors such as the size of the clot, the location of the clot, and individual variations.
Prompt medical attention is crucial to prevent complications. If you experience symptoms such as sudden shortness of breath, chest pain, or rapid heart rate, it is important to seek immediate medical care. Early diagnosis and treatment can help prevent a life-threatening condition known as pulmonary embolism.

Understanding the timeframe for a blood clot to travel from the leg to the lungs highlights the importance of early intervention. By recognizing the symptoms and seeking medical help promptly, individuals can minimize the risk of complications and improve their chances of a positive outcome.
If you have concerns about blood clots or suspect you may have one, do not hesitate to reach out to a healthcare professional. They can provide a proper diagnosis and recommend appropriate treatment options based on your individual circumstances.
Treatment Options for Blood Clots in the Lungs
Treatment for blood clots in the lungs, or pulmonary embolism, encompasses various medical interventions to address the condition and prevent further complications. The specific treatment approach depends on the individual’s condition and the severity of the blood clot.
1. Anticoagulant Medications
Anticoagulant medications are commonly prescribed to individuals with blood clots in the lungs. These medications work to prevent further clot formation and allow the body to naturally dissolve the existing clot over time. Commonly used anticoagulants include:
- Warfarin
- Heparin
- Direct oral anticoagulants (DOACs) such as apixaban, rivaroxaban, dabigatran, and edoxaban
2. Thrombolytic Therapy
Thrombolytic therapy may be considered in cases where there is a need to dissolve the blood clot more rapidly. This treatment involves the administration of medications that can break down the clot, facilitating its removal from the lungs. Thrombolytic therapy is typically reserved for severe cases or situations where there is a high risk of further complications.
3. Surgical Procedures
In certain severe cases of blood clots in the lungs, surgical interventions may be necessary. One such procedure is the placement of a filter in the large vein in the abdomen, known as the inferior vena cava (IVC). This filter is designed to catch clots and prevent them from reaching the lungs, reducing the risk of pulmonary embolism.
4. Alternative Medical Interventions
While anticoagulant medications, thrombolytic therapy, and surgical procedures are the mainstay of treatment for blood clots in the lungs, other alternative medical interventions may be considered in specific cases. These alternative interventions include:
- Thrombectomy: A procedure that involves the removal of the blood clot using specialized catheters or surgical techniques.
- Catheter-directed thrombolysis: A minimally invasive procedure where a catheter is used to deliver clot-dissolving medications directly to the site of the clot.
It is important to consult with a healthcare professional to determine the most appropriate treatment option based on individual circumstances.
Preventing Blood Clots
Preventing blood clots is crucial to maintaining overall health and reducing the risk of serious complications. By implementing certain measures, individuals can take proactive steps in reducing blood clot formation and minimizing the chances of developing thrombosis.
1. Staying Active
Regular physical activity plays a vital role in preventing blood clots. Engaging in moderate-intensity exercises, such as brisk walking, cycling, or swimming, helps promote blood circulation and prevents blood from pooling in the veins. Incorporating at least 150 minutes of aerobic activity per week can significantly reduce the risk of clot formation.
2. Maintaining a Healthy Weight
Excess weight can put strain on the body’s cardiovascular system, increasing the risk of blood clot formation. By adopting a healthy diet and engaging in regular exercise, individuals can maintain a healthy weight and reduce the likelihood of developing blood clots.
3. Quitting Smoking
Smoking is a significant risk factor for blood clot formation. Chemicals found in cigarettes can damage blood vessels, leading to clotting. Quitting smoking not only reduces the risk of blood clots but also improves overall cardiovascular health.
4. Managing Underlying Medical Conditions
Certain medical conditions, such as heart disease, cancer, and autoimmune disorders, can predispose individuals to blood clots. By effectively managing these conditions with the help of healthcare professionals, individuals can reduce the risk of clot formation.
5. Medications for High-Risk Individuals
For individuals at high risk of blood clots, preventive medications may be prescribed. Anticoagulants, such as warfarin or heparin, can help prevent clot formation and reduce the risk of thrombosis. It is important to follow medical advice and regularly monitor these medications to ensure optimal effectiveness.
6. Healthy Lifestyle Choices
In addition to the above measures, maintaining a healthy lifestyle can further contribute to blood clot prevention. This includes eating a balanced diet rich in fruit and vegetables, and whole grains, reducing alcohol consumption, and staying hydrated.
| Preventive Measures | Benefits |
|---|---|
| Staying active | Improves blood circulation and prevents blood pooling in the veins |
| Maintaining a healthy weight | Reduces strain on the cardiovascular system and lowers the risk of clot formation |
| Quitting smoking | Reduces the risk of blood vessel damage and improves overall cardiovascular health |
| Managing underlying medical conditions | Reduces risk factors associated with clot formation |
| Medications for high-risk individuals | Prevents clot formation and reduces the risk of thrombosis |
| Adopting a healthy lifestyle | Supports overall cardiovascular health and reduces the risk of clot formation |
By taking these preventive measures, individuals can significantly reduce their risk of developing blood clots. However, it is essential to consult with healthcare professionals for personalized advice and guidance based on individual health conditions and risk factors.
Conclusion
Blood clots are a serious medical condition that can be life-threatening if not treated promptly. It is crucial to understand the risk factors and recognize the symptoms to ensure early diagnosis and intervention. Seeking immediate medical attention is essential.
The speed at which a blood clot travels from the leg to the lungs can vary. However, prompt treatment can help prevent complications and reduce the risk of death. Taking preventive measures, such as staying active and managing underlying medical conditions, can also help reduce the risk of blood clot formation.
It is important to prioritize your health and seek appropriate medical care if you have concerns about blood clots. By being aware and proactive, you can take steps to prevent blood clots and ensure your well-being.
FAQ
1. How fast does a blood clot travel from the leg to the lungs?
The speed at which a blood clot travels from the leg to the lungs can vary and depends on various factors. In some cases, a blood clot can reach the lungs within hours or days, while in other situations, it may take longer. It’s crucial to seek immediate medical attention if you suspect a blood clot to minimize the risk of complications.
2. What is deep vein thrombosis (DVT) and how long does it take for a blood clot to reach the lungs?
Deep vein thrombosis (DVT) is a condition where a blood clot forms in a deep vein, typically in the leg. The time it takes for a blood clot to reach the lungs can vary and depends on multiple factors. While it can happen relatively quickly, it’s essential to recognize the signs and symptoms of DVT to seek early intervention and prevent the clot from reaching the lungs, causing a pulmonary embolism.
3. What are the symptoms of deep vein thrombosis (DVT) and pulmonary embolism (PE)?
The symptoms of DVT may include swelling, pain, warmth, and redness in the affected area, often the leg. On the other hand, symptoms of pulmonary embolism (PE) may include sudden shortness of breath, chest pain, rapid heart rate, coughing up blood, and lightheadedness. It’s crucial to seek medical attention immediately if you experience any of these symptoms.
4. How are DVT and PE diagnosed and treated?
The diagnosis of DVT and PE involves various tests, including ultrasound, blood tests, and imaging scans. Once diagnosed, treatment options may include blood-thinning medications, such as anticoagulants, and interventions, such as thrombolytic therapy or surgical procedures, depending on the severity. Prompt diagnosis and appropriate treatment are essential to prevent complications and protect against further clot migration.
5. What can influence the speed at which a blood clot travels from the leg to the lungs?
Several factors can affect the speed at which a blood clot travels from the leg to the lungs. These factors include the size of the clot, its location within the deep veins, and individual characteristics, such as overall health and activity levels. It’s important to be aware of these factors to understand the potential risks and take appropriate preventive measures.




